We regularly highlight the outstanding quality improvement (QI) work of many general practices in our region. To close off what has been another huge year for the sector, we want to show you how we support this work.
But, first, let’s pay tribute to the collective QI efforts of practices across Melbourne’s centre, north and west. It’s now official: you are raising the bar for primary care.
Latest PIP QI data report shows continued improvement
Last year, the Australian Institute of Health and Welfare (AIHW) published its Practice Incentives Program Quality Improvement Measures: National report on the first year of data 2020-21. The report brought together de-identified data collated by primary health networks (PHNs) from more than 5,700 Australian general practices. The data described 10 measures that empower our understanding of population health.
At the time, while practices had made significant improvements in many areas, our region ranked lower than the national average. This was understandable given the size and diversity of the catchment, the population health challenges we face, and the fact that the area was the hardest hit by COVID-19 during the first two years of the pandemic.
Our Chief Executive, Christopher Carter, said at the time that “the data shows that while many improvements have been made, many more are possible – and necessary for the future health of our growing region.”
Twelve months on, we are pleased to report that more improvements are indeed happening. The AIHW’s 2021-22 report shows that practices in our region have collectively improved on 8 out of 10 measures. They also now rank above the national average on the eighth measure: the proportion of patients with the necessary risk factors assessed to enable cardiovascular disease assessment.
Chris Carter notes: “The result I think has two drivers: the variety of high quality improvement options that NWMPHN provides, and the enthusiasm with which general practices embrace them.
“This year the data shows we are on the right track, but there is still much room for improvement.”
How QI drives our vision for primary care
Our Primary Health Care Improvement Team shares a passion for supporting better care in general practice. Its members have worked with practices for a long time and understand the challenges primary care providers face. We do our utmost to support each of the 550+ practices in our region, because we believe in our vision for a primary care system that is person-centred, comprehensive, coordinated, accessible, high-quality and safe.
The AIHW results are encouraging, and show that we are improving, step by step. (Or, PDSA cycle by PDSA cycle!)
Each quarter, the team prepares a comprehensive internal report that shows how we are working with practices to achieve this vision. We look at the data and take stock of what’s working, discuss how we can improve and plan our work for the next quarter. We also look at the feedback we receive from the sector, and workshop how to act on it.
This guides our role as a capability builder, a communicator, a commissioner, a champion and a coordinator. Or, as we refer to them internally, “the 5Cs”.
Here is an outline of how this framework is driving our QI process and contributing to the work happening on the ground in general practice.
Capability builder
We support practices to achieve results like those highlighted in the AIHW report by ensuring they have access to the best possible education, QI tools, and resources including HealthPathways Melbourne.
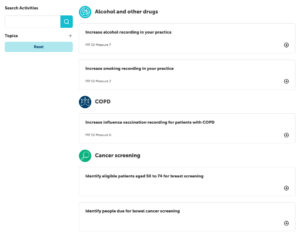
This year we launched our QI activity hub, giving practices access to localised, practical templates to improve patient outcomes and deliver best practice care. Practices downloaded these more than 400 times, and we are adding new ones regularly.
Communicator
We deliver timely and relevant localised information to health care providers so they can respond to emerging trends and patient needs. We also create community awareness campaigns and consumer resources that increase access to and awareness of existing and new health services.
This year we stayed in touch regularly with primary care providers through our e-newsletters, including more than 100 COVID-19 updates and other bulletins. We also implemented large public awareness campaigns that helped more than 100,000 patients receive care through our GP respiratory clinics, and thousands of others receive pre-infection winter treatment plans.
Commissioner
We commission and co-design local and regional solutions to address service gaps, better integrate health care and ensure equitable access.
This year, with lockdowns a thing of the past and COVID-19 spreading easily through our community, we knew that general practices had their work cut out protecting those most at risk. So, we designed and implemented the Proactive Engagement Project, which offered financial incentives to practices to increase uptake of COVID-19 and influenza vaccinations, and boost early assessment and treatment for COVID-19.
More than 100 practices jumped at the chance, leading to more than 11,000 COVID-19 and influenza vaccinations that otherwise would not have been given, saving thousands of people from serious illness and possibly death. The recently released project summary (.pdf) also shows that more than 20,000 at-risk patients were screened, and close to 5,000 winter preparedness plans were completed, giving eligible patients quick access to antiviral medication should they become infected with COVID-19.
The success of this project is now informing our planning for winter 2023 – watch this space.
Champion
We regularly advocate for primary care as the foundation for a high-performing and sustainable health system. Our General Practice Advisory Group and Clinical and Community Councils are crucial for informing these advocacy efforts. We acknowledge that system-wide investment and policy change are sorely needed, as many practices face staff shortages, burnout and rising costs.
To that end, we were pleased to host the Hon Ged Kearney, Federal Member for Cooper and Assistant Minister for Health and Aged Care, at our recent women’s health forum. Herself a former nurse, Minster Kearney’s passion for and working knowledge of the health sector were impressive. It is encouraging that system change is being driven by people who understand the issues so deeply.
You can watch our forum with Minister Kearney on our website.
Coordinator
We foster strong partnerships and collaborations across local, state and federal governments – between primary health, acute and specialist services.
Most recently, this work is exemplified by our statewide role in coordinating the Victorian Government’s investment in GP respiratory clinics and priority primary care centres. Our work with the advisory groups for these initiatives, along with their respective communities of practice, is ensuring that more Victorians get the right care, in the right place, at the right time.
Much is still to be done, but the data show we are headed in the right direction. Bring on 2023!