
By Dr Jeannie Knapp, GP and Primary Health Care Improvement GP Adviser, North Western Melbourne Primary Health Network.
What is family violence?
Anyone can be affected by family violence, regardless of their age, gender, sexual identity, cultural background, ability, religion, wealth, status or location.
Women are statistically more likely to be victims of family violence. Family violence directly affects one in five Victorian women over the course of their lifetime. It is the leading contributor to preventable death, disability and illness in Victorian women aged 15 to 44 years.
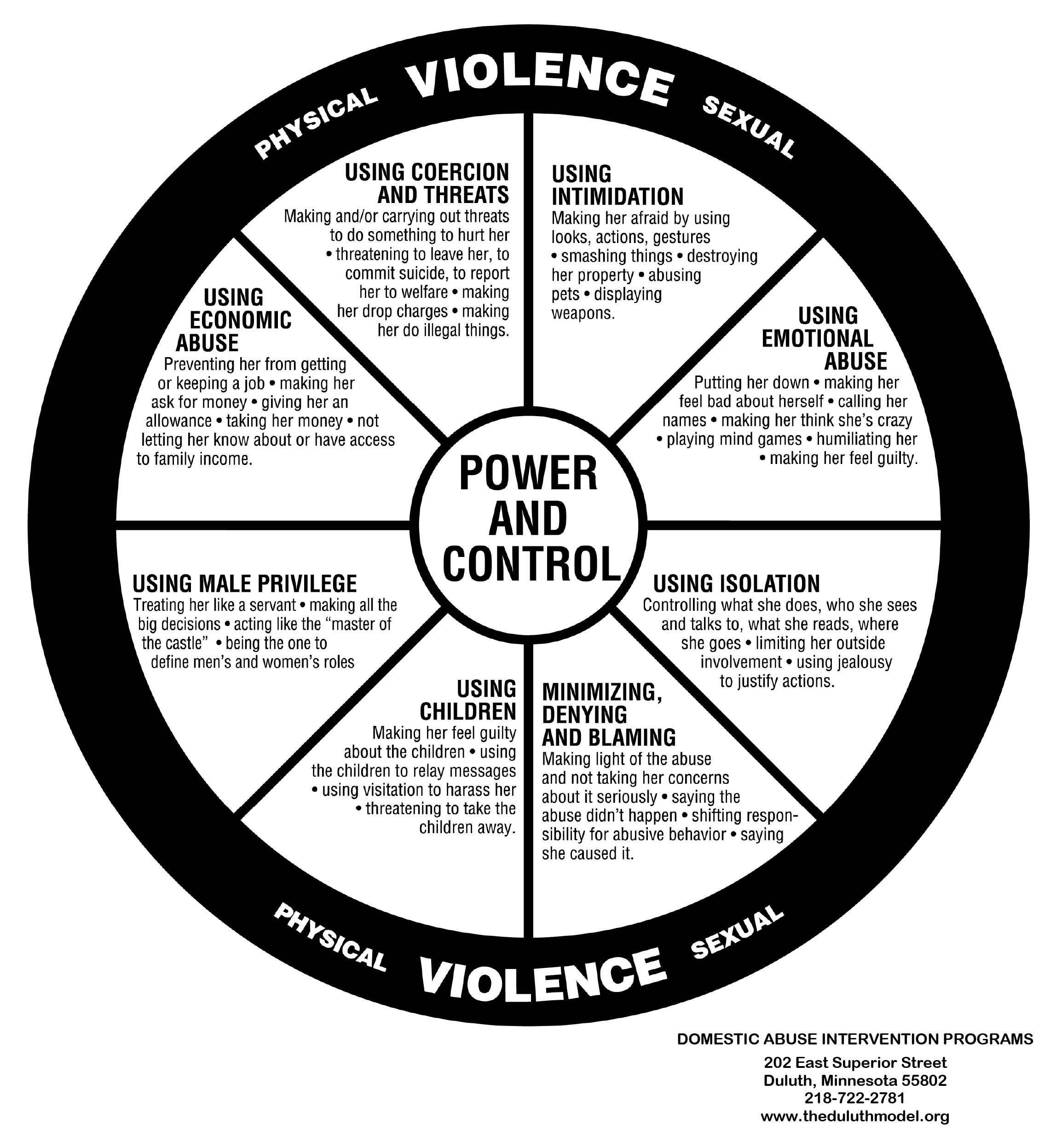
Family violence covers a range of behaviours committed by a person against a family member. All the behaviours aim to control a family member through fear, and include the following:
- physical abuse, for example pushing or hitting
- sexual abuse, including forcing a person to have sex or engage in sexual activity
- emotional or psychological abuse, including calling the person by names and controlling their behaviour
- intentionally damaging a family member’s property
- economic abuse – this includes controlling a family member’s bank accounts and money without their consent
- any other behaviour that causes the family member to feel fear for their safety, the safety of another person or an animal
- if a child hears, sees or is exposed to the effects of family violence
Threatening to do any of the above is also classified as family violence.
Have family violence rates increased during lockdown?
COVID-19 lockdown conditions have unfortunately increased the likelihood of family violence. Increased isolation, often with the abuser, and being away from support and help-seeking networks can increase the risk of abuse. The pressures of being stuck at home together with little respite puts additional pressure on families. Increased financial distress and unemployment can also be triggers, as can increased alcohol use.
Reports indicate that family violence rates have increased worldwide during the lockdown. Speaking to the ABC’s Rachel Clayton, St Vincent’s Hospital’s chief social worker, Lisa Braddy said presentations to the hospital related to family violence had more than doubled in the first quarter of 2020 compared to 2019.
“We have seen a decrease in overall emergency department presentations but family violence disclosures have increased considerably since the same time last year in terms of proportions and figures,” Ms Braddy said.
While to date there is no data specific to general practice, if emergency department presentations have increased then presentations to general practice may also increase. There have been reports that incidences tripled in parts of China during the country’s isolation period.
What can we do in general practice?
Health practitioners are the professionals most often told about family violence, even more so than police. Studies show abuse is associated with depression, anxiety, other psychological disorders, drug and alcohol abuse, sexual dysfunction, functional gastrointestinal disorders, headaches, chronic pain and multiple somatic symptoms. Sexual abuse has also been linked with chronic pelvic pain.
GPs can identify predisposing risk factors, noting early signs and symptoms of violence. Evidence shows women are open to being asked about their safety at home.
Some possible questions to ask and statements to make if you suspect intimate partner abuse include:
- Are you afraid of your partner? Have you ever been afraid of any partner?
- Has your partner ever controlled your daily activities, or do they constantly put you down?
- Has your partner ever physically threatened to hurt you?
- Has your partner pushed, kicked, slapped or otherwise hurt you?
- Sometimes partners react strongly in arguments and use physical force. Is this happening to you?
- Have you ever felt unsafe in the past?
I ask a lot of my patients about abuse because no one should have to live in fear of their partners. GPs can play an important role by providing a first-line of response and offering referral pathways and evidence-based patient resources.
How to manage disclosure
Referral or connection to specialist services should be offered if disclosure occurs.
If a patient does disclose, they may not yet be ready to access services. In this case, it is important to validate their experience with statements such as:
- Everyone deserves to feel safe at home.
- You don’t deserve to be hit or hurt, and it is not your fault.
- I am concerned about your safety and wellbeing.
- You are not alone. I will be with you through this, whatever you decide. Help is available.
An initial assessment should also be made of the patient’s safety. This may be as simple as checking if it is safe for the patient (and their children) to return home. A more detailed risk assessment can be done at a subsequent visit and include questions about escalation of abuse, the content of threats, and direct and indirect abuse of any children.
HealthPathways Melbourne
Access the Family Violence pathways on HealthPathways Melbourne.
Don’t have a login? Request access here.
Resources for people who have experienced family violence
- Australian Department of Human Services: Family and domestic violence
Phone: 132 850 (Information in different languages and translation services are available) - National Sexual Assault Domestic Violence Counselling Service (includes translator services)
24/7 phone line: 1800RESPECT - White Ribbon’s list of hotlines and support services
- inTouch – Multicultural Centre Against Family Violence
- Safe Steps Family Violence Response Centre
24/7 Victorian family violence response phone service: 1800 015 188 - withRespect – LGBTIQ family violence service: 1800 542 847 (1800 LGBTIQ)
Resources for health professionals
- RACGP White Book: Abuse and Violence, Working with our Patients in General Practice (4th edition)
- Melbourne Medical School learning module: Identifying and Responding to Domestic Violence
- Domestic Violence Resource Centre Victoria Guide for General Practitioners
To learn more about the role of primary care professionals and how to respond to family violence, visit the family violence for primary care page. This page includes family violence services and other resources including a short video Starting Conversation About Family Violence by Professor Kelsey Hegarty of the University of Melbourne.
2022 Community of Practice: Family Violence sessions
To take part in the 2022 Community of Practice: Family Violence sessions, register below:
Areas: Brimbank, Hobsons Bay, Maribyrnong, Melton, Moorabool and Wyndham
Areas: Darebin, Hume, Macedon Ranges Melbourne, Moonee Valley, Moreland and Yarra.





