By Dr Jeannie Knapp, GP and Primary Health Care Improvement GP Adviser, North Western Melbourne Primary Health Network.
What is the Quadruple Aim?
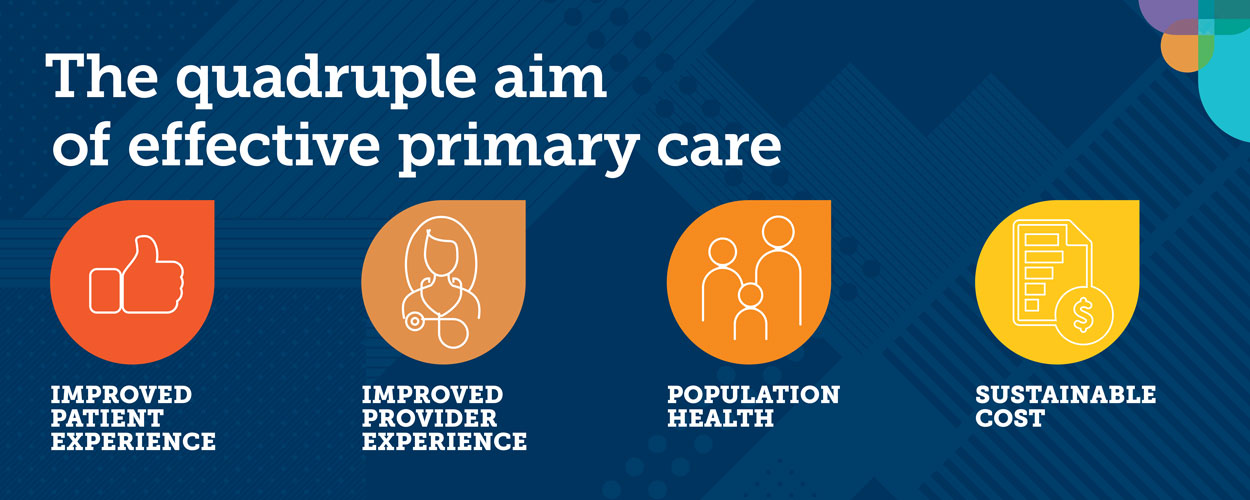
The quadruple aim is a framework to guide us towards the outcomes we should be aiming for with improvement activities in primary care. It was identified through extensive primary care research – initially as the triple aim, then refined to the quadruple aim.
Effective high-quality practices look to make improvements in all four areas – improved patient experience, improved provider experience, improved population health – at a sustainable cost.
When we discuss quality improvement and undertake quality improvement activities, we often tend to focus on improved patient outcomes. However, a well-run, high-quality practice will also improve income and reduce costs.
How quality improvement activities can improve practice income: A personal example
In my own practice, we acknowledged that our patients with diabetes were all too often receiving care on an ad hoc basis. Every doctor was approaching the annual check differently and were often feeling overwhelmed by requests for diabetes check-ups on top of other presentations. We had poor systems in place to support reminders for check-ups and pre-check-up blood work.
We made a conscious effort to invest protected time to create a database of patients with diabetes, educational updates for clinical staff and to streamline patient care with more proactive reminders for blood tests and annual check-ups. The investment has paid off, as we have significantly improved the proportion of our patients with recorded HbA1c% and ACR results (improved population health).
We have also increased our income: by increasing routine appointments, yes, but predominantly by increasing chronic care item claims (sustainable cost). Providers have reported more satisfaction from performing diabetes care in a more planned way (improved provider experience). Patients have also enjoyed more structured care, and we have offered the annual check-up for free (improved patient experience).
Some other examples in my practice include:
- Recalling patients for 45-49-year-old checks (Medicare health assessment item number)
- Using Topbar to identify patients at risk of osteoporosis and arranging review and bone density measurement (GP management plan)
- Recalling patients with COPD for an annual check-up and action plan review (GP management plan +/- spirometry)
How you can embed continuous quality improvement it your practice
Effective high-quality practices embed quality improvement (QI) into the day-to-day running of the practice, informing all decisions. Evidence shows that improvement is most likely when all staff support change, so adopt a whole-of-team approach from the outset.
Starting small is key, with change broken down into manageable pieces. Within your practice, this not only helps to reduce clinical and administrative risks, but also to foster unity within the practice team and avoid resistance to change. Proven changes can then be implemented more widely across the practice, while refined or new ideas can also be tested.
Here are some tips to help you get started or improve your QI processes:
- Develop a QI strategy for your practice; create a QI team, appoint a QI clinical lead and (ideally) provide them with some protected time
- Do some staff training on using the model for improvement (available in our QI Toolkit)
- Use data to guide you to priority areas
- Use the quadruple aim as a checkpoint for all quality improvement activities
- Share widely with the team – celebrate your wins and learn from your losses! Keep the conversation going and everyone involved
How can the PHN team help?
North Western Melbourne Primary Health Network (NWMPHN) is committed to supporting general practices on their quality improvement journey. As you are aware, in order to the claim the Practice Incentives Program Quality Improvement (PIP QI) Incentive, your practice must be undertaking QI in conjunction with NWMPHN. While PIP QI requires reporting against on the 10 improvement measures, you are not restricted to using these 10 measures for your own QI goals.
There are several NWMPHN resources available to assist you:
- NWMPHN has developed the Quality Improvement Guide and Tools, which we highly recommend reading first. It’s a great starting point before embarking on a QI process. It includes many practical examples, as well as an explanation of the Model for Improvement.
- NWMPHN’s General Practice Improvement Plan is a resource practices can use to identify specific priorities and objectives that they would like to achieve over 12 months and outlines how the PHN will work with you. Relationship Managers – each practice in the NWMPHN catchment has their own relationship manager and can provide further support on implementing continuous quality improvement in your practice. Contact them by email: primarycare@nwmphn.org.au
- NWMPHN’s Team Health Check PDSA (.docx) and the Improvement Foundation’s Team Health Check Score Sheet (.docx) can help you assess your team culture and identify roles and responsibilities. Along the way, you may also identify team members who might resist change, as well as potential issues or matters to address before your project begins.
- NWMPHN has developed a suite of QI workbooks on a variety of different topics to give you practical advice and guidance on QI projects including a workbook focusing on the PIP QI improvement measures.
- NWMPHN can assist you with installing and training for CAT4 – a data aggregation tool.
- NWMPHN has developed PIP QI benchmarking reports. Read our article to learn more about these reports and how they can help your practice.




