
By Dr Jeannie Knapp, GP and Primary Health Care Improvement GP Adviser, North Western Melbourne Primary Health Network.
Background
Preventative activities and screening are an integral part of general practice. Detecting problems early can lead to better outcomes.
The leading causes of death and disability in Australia are preventable or able to be delayed by early treatment and intervention. The RACGP Red Book is considered the gold standard for preventative activities in general practice.
Australia has one of the best cancer survival rates in the world. There several factors to this success but it can partly be attributed to well-funded and organised cancer screening programs and access to high quality care. Australia also has one of the lowest rates of cervical cancer in the world; again, this is largely due to the national cervical cancer screening program and the human papillomavirus (HPV) vaccination program.
Patients are not accessing care
The number of patients accessing services is down across the sector. There are reports that:
- General practices have fewer patients attending and many are delaying screening
- Pathology companies are receiving up to 40 per cent less requests for testing, including screening and routine monitoring tests. For example: HbA1c percentage
- Emergency departments are seeing fewer presentations for acute problems such as heart attacks and strokes.
Peter MacCallum Cancer Centre has reported an approximate 20 per cent reduction in both referrals and patients attending routine treatments and appointments during the pandemic. Some anecdotal estimates are as high as a 50 per cent reduction in access to some health care services.
This suggests patients who need care are not receiving it. Patients may not be attending because they fear for their safety or they do not wish to burden the health system.
Some practices have ceased screening and routine care because they believe resources ought to be focused elsewhere, that patients should not be encouraged to leave their homes or that referrals to hospitals might not be safe. This could lead to a significant risk that cancers are at a more advanced stage when they are diagnosed and an increased number of preventable deaths.
Attending a medical appointment is one of only five allowable reasons to be out of your home during the lockdown in Victoria. The Victorian Department of Health and Human Services’ advice is that we should “encourage patients to continue to proactively manage chronic illnesses, take routine tests and attend health services”.
Could delaying care kill more Australians than COVID-19?
At the time of writing 100 people have died in Australia from the coronavirus. Many commentators believe that there is a potential for more people to die from delayed routine care, preventative activities, screening and delayed diagnoses than from COVID-19.
Associate Professor Dion Stub, an interventional cardiologist and medical advisor to Ambulance Victoria, told newsGP recently: “We’ve had so few deaths from COVID-19 that we may have more from preventable illnesses, from malignancies to heart disease.”
Potential for a post-COVID-19 tsunami
Delaying referrals now to ease the burden on our health system may actually increase the burden after the pandemic ends or is brought under control. Public hospitals and private specialists are mostly fully staffed and operating normally. The coronavirus outbreak hasn’t been as severe here as overseas and our health services are not overburdened. However, delayed screening and diagnosis now may lead to more complex and advanced problems later.
Business as usual
Ideally you should adopt a business as usual approach with your patients. If possible, reach out to your patients and reassure them that it is OK to attend for appointments like cervical screening, blood tests or vaccinations.
You could use email, social media, your practice’s website or SMS to communicate this vital message to patients. Continue to use your reminder and recall system to recall patients for routine screening, preventative activities and routine care. Continue to send referrals as per your usual practice. All public hospitals in the North Western Melbourne Primary Health Network (NWMPHN) region are accepting routine referrals.
You might like to consider reaching out to patients who have delayed their care. They may not know they can use telehealth or simply need to be reassured that it is OK. Talk to your patients who need specialist care about the measures you’ve put in place to ensure their safety. These measures might include telehealth consultations, physical distancing, hygiene practices and temperature screening. We are all craving human connection during the pandemic and a reassuring chat can go a long way.
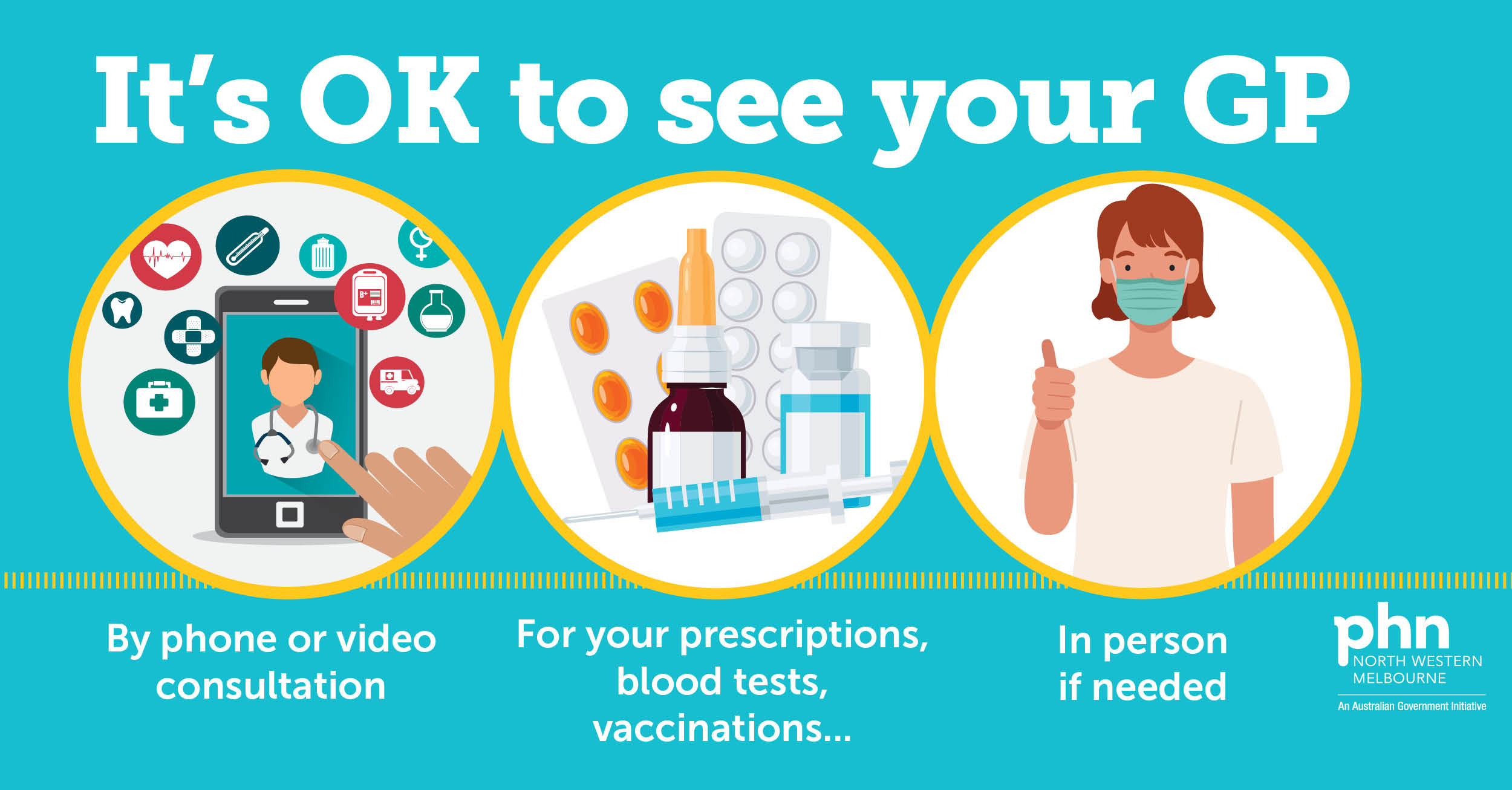
NWMPHN have developed the It’s okay to see your GP campaign to encourage people to stay in touch with their GP. Advertisements are running in newspapers and on social media throughout our region. You might like to consider using this campaign on your website or in other communications with patients – visit nwmphn.org.au/seeyourGP for more information.
It’s an old adage in medicine that prevention is better than cure – and this continues to hold true during the coronavirus pandemic.
HealthPathways Melbourne 
Check the COVID-19 Impact on Local Services page to see the latest changes and updates to patient referrals into local health district services.
Use the following cancer screening pathways for evidence-based advice:
- Breast Cancer Screening
- Prostate Cancer Screening
- Cervical Screening
- National Bowel Cancer Screening Program (NBCSP)
Need a login? Request access here or contact info@healthpathwaysmelbourne.org.au




