A new Victorian Department of Health policy to streamline access to non-admitted specialist services in public hospitals, to be phased in over the next two years, will make the process easier for patients and the GPs who refer them.
Non-admitted hospital services are provided to public patients in a range of settings. These patients do not undergo a formal admission process and do not occupy a hospital bed.
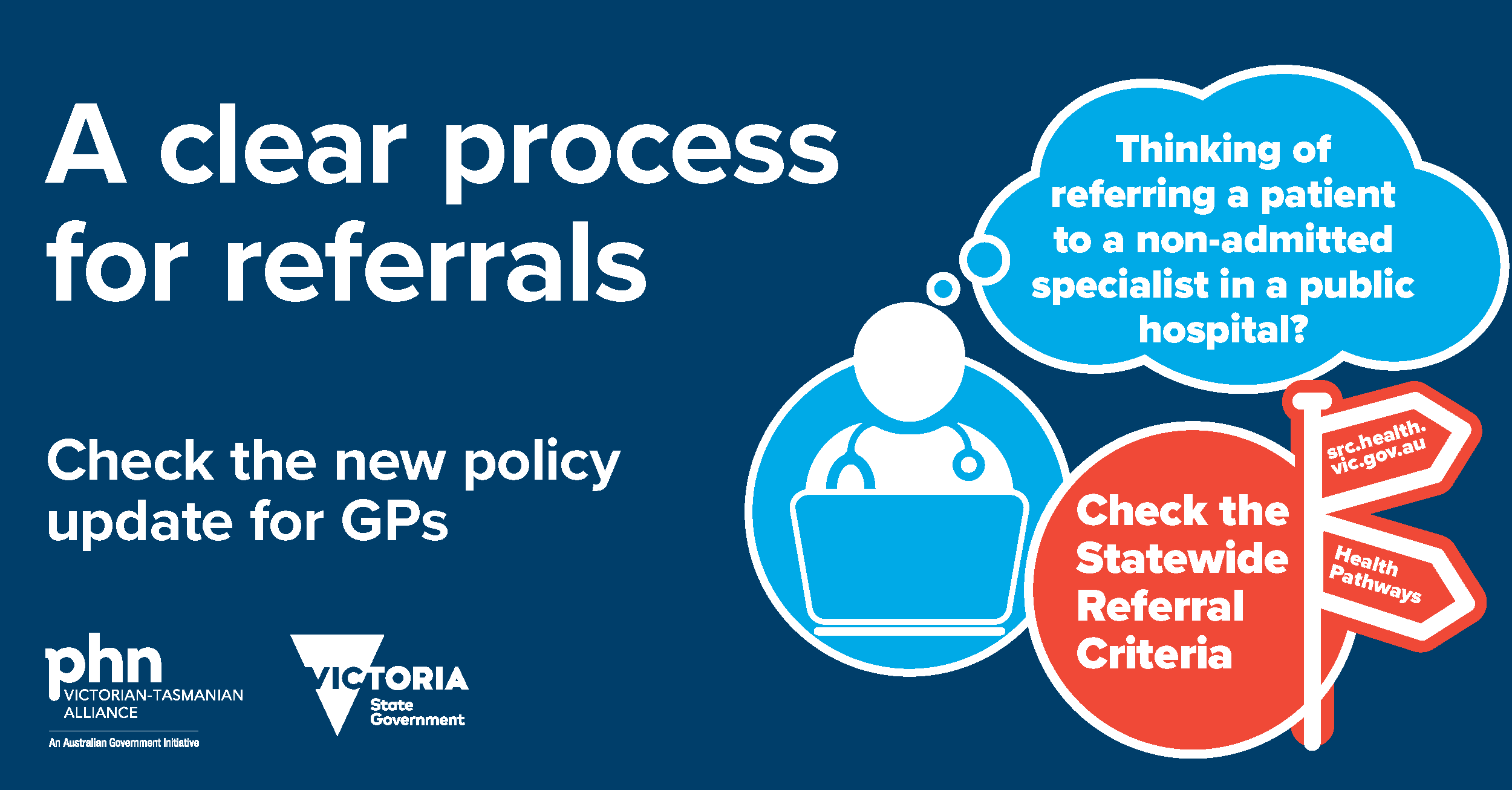
In the past there has sometimes been confusion around the requirements and responsibilities of GPs, specialists and hospitals in governing this process. Following a review of non-admitted service referral protocols this has now been resolved, with clear guidelines established. The result, called the Managing referrals to non-admitted specialist services in Victorian public health services policy, is the first major overhaul of the system in a decade.
The new policy provides simple and clear pathways for Victorian public health services and referring GPs.
Health services can request a specialist be named in referral documents; however, it is no longer a reason for rejecting a referral. The policy also commits hospitals to informing GPs about their referrals within 8 working days.
“This policy provides a level of assurance that we haven’t had before for non-admitted patients,” said Dr Jeannie Knapp, a GP advisor to North Western Melbourne Primary Health Network.
“Victorian hospitals already provide these levels of communication for surgery, and most hospitals have this referral management in place. As a GP, it is reassuring that there is now a process of clear communication in place.”
Dr Knapp added that as new directives in the policy come into effect over the next two years they will have a positive impact for doctors and consumers.
“Knowing that my patients are informed of waiting times allows me to better support them over this time,” she said.
“Having this transparency reduces stress and anxiety for both me and the patient.
“I still regularly check HealthPathways to ensure I have all the details needed for a referral – so it is accepted the first time. And in a perfect world there’d be a universal e-referral system for all hospitals. However, I feel better knowing that if I make an error on an urgent referral, the hospital will phone me to follow up and ensure the patient doesn’t fall through the cracks.”
For more detail on the implications of the new policy see here.




