
This was written by Dr Scott Parsons for NWMPHN.
Sara is a first-time mother to 16-month-old toddler Tara. Sara takes her daughter to see their GP following an 8-month history of constipation.
Sara’s GP consults the Constipation in Children pathway as s/he has limited experience managing this condition in a child this young.
Sara’s GP begins the consult by taking a history and discovers that
- When Tara was 10-months, Sara’s breast milk supply diminished, and Sara was incorrectly advised it was safe to go straight to cow’s milk.
- Previous advice had been to increase fluids and fibre to relieve Tara’s constipation. No medications had been suggested.
- Sara is having lots of mealtime issues, with Tara refusing age-appropriate food. She is currently on 3-4 bottles per day of cow’s milk. Each bottle is approximately 200mls.
The GP’s physical examination reveals Tara is an otherwise healthy active toddler, recording a weight of 11.6kgs (75th centile) and a height on 50th centile. The findings from the initial assessment indicates excessive and early cow’s milk ingestion resulting in:
- Functional constipation
- Risk factor for Fe deficiency +/-anaemia
To address the functional constipation, the GP refers back to the Constipation in Children pathway, which advises lessening cow’s milk consumption and commencing high dose osmotic laxative.
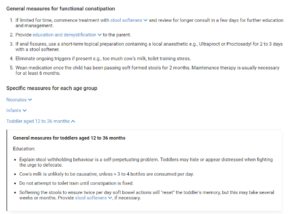
The GP confidently prescribes Tara stool softeners using the information provided in the pathway (stool softener drop down, image below) and advises Sara how to wean the medication down to a medication dose until Tara has soft bowel actions and is a ‘happy pooer’.

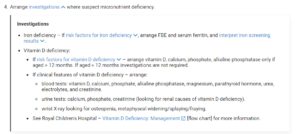
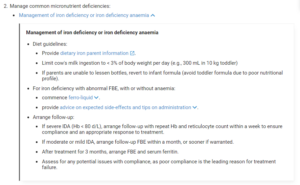
The GP then consults the Infant and Toddler Nutrition and Feeding Concerns pathway to address the suspected Iron deficiency +/- anaemia as a result of excessive cow’s milk consumption and is advised to arrange a full blood count and serum ferritin to confirm diagnosis.
To complete the consult, the GP sends Sara useful patient resources from both pathways, including the Raising Children Network Toddlers Nutrition and Fitness patient resource for her to look over and refer to following the appointment.
A few days later
The GP receives the results of Tara’s blood test which show:
- Tara has Fe Deficiency Anaemia
- Tara’s Hb was 88 d/L with microcytic microchromic picture and low serum ferritin.
Upon receipt of these results, the GP returns to the Infant and Toddler Nutrition and Feeding Concerns pathway and decides to commence ferro-liquid 6mls daily and provide tips on administration and arrange repeat blood tests in one month.
Follow up appointment, one month later.
The GP finds Tara’s Hb has improved, and her serum ferritin is normal. After checking the pathway, the GP decides to continue serum ferro-liquid for three months with another blood test at the time.
Tara has loose stools though is still oppositional to opening her bowels. The GP advises Sara to continue the osmotic laxative and only wean when she appears to have no residual apprehension to opening her bowels.
Lessening cow’s milk and improving mealtime experiences has improved Tara’s diet significantly.
Note from the Editor:
Excessive cow’s milk is the most common dietary factor in constipation and can also lead to Iron deficiency. This is particularly so when there is a history of exclusive breastfeeding. Cow’s milk has no iron content and, in some cases, can result in an essentially asymptomatic protein enteropathy leading to occult blood loss. It is not uncommon for toddlers to present with Hb as low as 5 -6 d/L before symptoms and signs of severe anaemia emerge.
Paediatric constipation guidelines do not recommend increasing fluids and fibre. Treatment with osmotic laxatives early and in appropriate dosages is the most effective management. The Infant and Paediatric HealthPathways have been adapted for the primary care context from the Royal Children’s Hospital Melbourne, Clinical Practice Guidelines.




