
By Dr Jeannie Knapp, GP and Primary Health Care Improvement GP Adviser, North Western Melbourne Primary Health Network.
Background
Cervical cancer is the 14th most common cancer affecting Australian women. The majority of cases are preventable with screening and appropriate treatment. While Australia has one of the lowest rates of cervical cancer incidence and mortality in the world, in 2017 participation in the National Cervical Screening Program was estimated at 54–56 per cent.
Lower participation in screening and higher rates of cervical cancer incidence and mortality have been reported in women with lower socio-economic disadvantage, women from culturally and linguistically diverse communities and Aboriginal and Torres Strait Islander women. Incidence of cervical cancer in Aboriginal and Torres Strait Islander women is more than two times that of non-Indigenous women, and mortality more than three times the non-Indigenous rate.
In December 2017, Australia transitioned from traditional cytology-based screening biannually (Pap smear) to a five-yearly human papillomavirus (HPV)-based screening program (CST).
Sources: Cancer Council Australia, Australian Institute of Health and Welfare.
Nurses and cervical screening in Australia
In Australia, GPs provide the majority of cervical screening. MBS data shows GPs provide 80 per cent of cervical screening, whereas in the United Kingdom female nurses perform 70–85 per cent of Pap smears. Many women prefer female practitioners to perform their CSTs. Of the GPs working in Australia in 2011, 43 per cent were women, whereas 90 per cent of nurses were women.
Evidence shows that nurses collect cervical screening tests of the same quality as doctors.
The traditional Medicare fee-for-service for a GP attendance funding model has limited the participation of general practice nurses in cervical screening.
Rationale for nurse-led cervical screening
Nurse-led cervical screening can improve access and continuity of care for patients for several reasons:
- Many women prefer a female practitioner to perform their CST
- Under-screened populations may feel more comfortable seeing a nurse for their CST
- Many patients feel more comfortable seeing a nurse. They may feel overwhelmed by the power dynamic that can occur in a GP/patient relationship. Patients sometimes talk more freely to nurses things about their lives, telling them important information because they don’t want to “bother” the GP (source).
- Nurses also take time to develop relationships with patients and nurses often maintain important organisational aspects of patient care, such as recall systems and follow up of specialist appointments (source).
Reduced workload for doctors
- Many studies have shown that doctors have high rates of burnout and psychological distress, depression and suicidality compared to other professionals. While not all of this relates to workload, workload is a contributing factor.
- Using a team approach within general practice can better utilise other team members and reduce the workload of GPs.
Improved job satisfaction for nurses
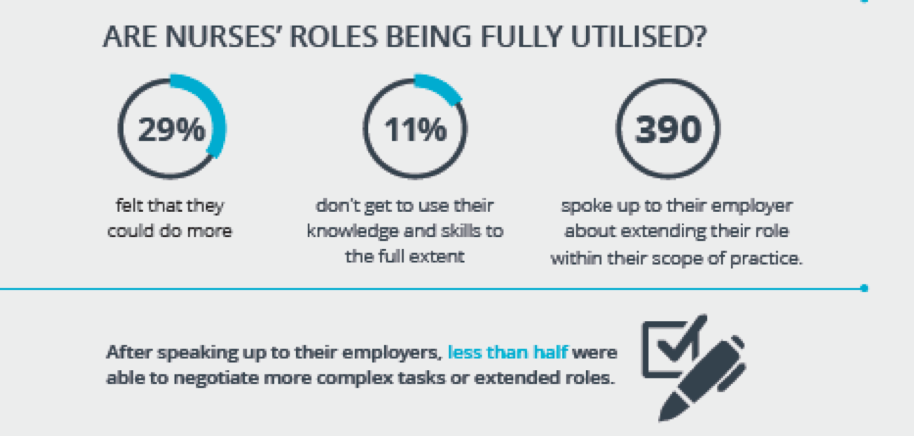
- In the Australian Primary Health Care Nurses Association workforce survey of 2017, 29 per cent of nurses felt they could do more than they currently were, 11 per cent felt they were not using their knowledge and skills to the full extent and 390 nurses had asked their employer to extend their role within their scope of practice. More than 50 per cent of employers had said no.
- With appropriate training, cervical screening is within the scope of practice for nurses in Australia.
- Extending scope of practice can significantly improve the job satisfaction for general practice nurses.
Thinking outside the box: Funding streams for nurse-led cervical screening
Below are some ideas about how you might fund nurse-led cervical screening:
- GPs are busy: A patient who sees the nurse rather than the GP tends to be replaced by another patient. Charging a small fee for the nurse to perform the cervical screening test is therefore a net increase in revenue, and reduced cost to the patient.
- Flow on patients: For some patients, access might be improved by seeing the nurse initially, which over time might lead to visits to the GP.
- Workforce Incentive Program (WIP) funding: Consider whether increasing a nurse’s hours in order to perform more nurse-led screening (either cervical or other) will also increase WIP payments.
- Chronic disease items: Use the-nurse led cervical screening to springboard into other care that the patient may need, which may generate income from chronic disease items.
- Health assessments: As outlined above, the screening test might be the entry point to identify health care needs and hence potential health assessments and related income.
More information 
- APNA Building Blocks: Explaining the essential elements of a nurse clinic
- APNA Nurse clinics: All you need to know
- Nurse-led clinics quality improvement toolkit (Hunter New England and Central Coast PHN)
- Larter: Funding to maintain employment of practice nurses during COVID-19
- Access the Cervical screening pathway on HealthPathways Melbourne. Need a login? Request access here.




