
Current events mean there are higher levels of distress in the community. Even the once simple act of catching a tram now provokes anxiety for many people. This is reflected in the number of patients seeking support through Head to Health.
Head to Health is an entry point into the mental health system but does not replace the central role a GP plays in looking after their patients’ mental wellbeing.
Head to Health can support GPs to manage the increasing number of people seeking mental health information and support, by assisting with navigating the service system and coordinating a comprehensive response where needed for patients.
So, how can you get the most out of Head to Health – and how does the intake team connect people with the best services for them?
In this article:
- Background
- What does Head to Health provide?
- How can GPs refer to Head to Health?
- How are Head to Health patients assessed to ensure equitable access to services?
- Where are the hubs – and what do they provide?
- What happens after you refer a patient?
- How should GPs decide whether to refer to Head to Health or CAREinMIND™
- What is the NWMPHN System of Care?
- Shared care survey for GPs
- More information
Background
Head to Health was established in Victoria in 2020 in response to the mental health effects of the COVID-19 pandemic. At the time it was known as HeadtoHelp; the name was changed in December 2021 as the Australian Government began rolling out the Head to Health mental health model across the nation. Currently it also operates in NSW and the Northern Territory.
This means the model is working. 92 per cent of people who accessed Head to Health to March 2022 showed an improvement in their mental health.
What does Head to Health provide?
In Victoria, Head to Health provides free advice and access to mental health care. It is backed by a statewide telephone intake service that anyone – patients, carers and clinicians – can access by calling 1800 595 212.
Head to Health intake is free. Following an initial assessment, Patients are then referred to and connected with the best available service, or combination of services. Many of these are also free. However, patients may also be referred to paid services if they have capacity to pay.
How can GPs refer to Head to Health?
A GP can refer anyone who has concerns about their mental health to Head to Health. The central intake team will work with the GP and the patient to refer them to the most appropriate services.
It is important to note that Head to Health is not a crisis service.
The current process for GP referrals into Head to Health is to phone the 1800 number while the patient is with you and provide general details. The intake clinician will then organise to complete the assessment with your patient at a time that suits them.
Alternatively, your patient is welcome to call 1800 595 212 so they can be assessed and navigated to an appropriate service.
The number is staffed Monday to Friday, 8:30am to 5pm.
If lines are busy, callers during these hours will have the option to leave a message and receive a call back.
How are Head to Health patients assessed to ensure equitable access to services?
The Head to Health intake team use the Initial Assessment and Referral (IAR) decision support tool. The IAR provides a standardised, evidence-based and objective approach to assist clinicians with determining the most suitable mental health care recommendations.
More information on the IAR tool is available in the IAR snapshot (.pdf). You can view the levels of care it determines in the image below.
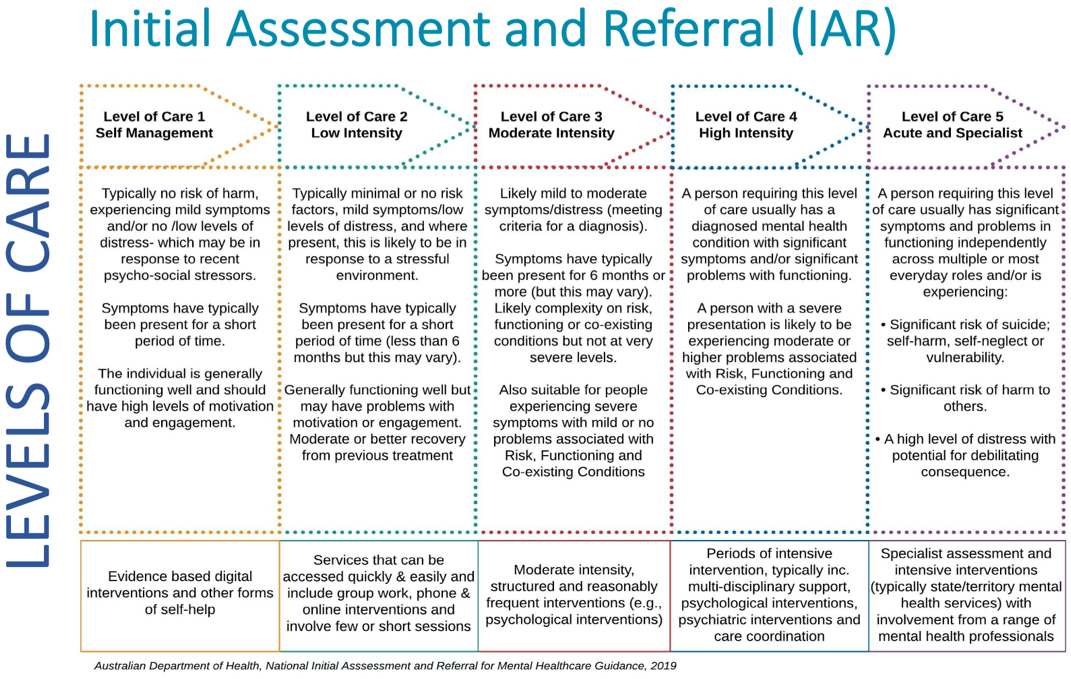
If a patient requires level 1 or 2 support as described in the IAR – GPs and the Head to Health intake team can point them to lower intensity services including evidence-based digital tools, or phone and online counselling options, like our CAREinMIND Wellbeing Support Service.
If a patient requires moderate to higher intensity support (level 3 or 4), they may be connected to one of the Head to Health hubs (see below), or to other services, including our CAREinMIND services and those run by other organisations.
HealthPathways Melbourne is another useful resource that can assist GPs with navigating the service system and referral requirements.
Where are the hubs – and what do they provide?
There are now Head to Health hubs in more than 20 locations across Victoria. In the North Western Melbourne Primary Health Network (NWMPHN) region, there are hubs in:
- Broadmeadows: run by DPV Health at 42/48 Coleraine Street, Broadmeadows
- Wyndham Vale: run by IPC Health at 510 Ballan Road, Wyndham Vale
- Brunswick East: run by Clarity Healthcare at 3/55 Nicholson Street, Brunswick East.
Hubs provide multidisciplinary teams including psychologists, mental health social workers, mental health nurses, care coordinators and support workers.
GPs should follow the referral process outlined above to determine whether a patient is suitable for care and treatment at a hub.
What happens after you refer a patient?
The central intake team will endeavour to inform you of the service that your patient is referred to, by faxing you a letter.
- People with level 1 and 2 needs will be connected to existing lower intensity services. (Around 11 per cent of callers to date have been assessed as level 1 or 2.)
- People with level 3 and 4 needs may receive care at the hubs, either onsite or through telehealth, or be referred to other more suitable services. (Around 87 per cent of callers to date have been assessed as level 3 or 4.)
- People with level 5 needs will be connected to specialist or acute mental health services, including emergency care or an area mental health triage. (Around 2 per cent of callers to date have been assessed as level 5.)
How should GPs decide whether to refer to Head to Health or CAREinMIND?
NWMPHN’s CAREinMIND services complement Head to Health. 
CAREinMIND might be a preferred option where a GP has undertaken an initial assessment and determined that their patient needs one of the following supports:
- Targeted Psychological Support
- Intensive Support for people experiencing more severe mental illness and needing clinical care coordination
- Suicide Prevention Support where someone has elevated risk of self-harm or suicide (but is not at immediate risk or in a crisis situation)
More information about the CAREinMIND services and referral process (including medical software compatible referral forms) is available on our website.
However, referring a patient to Head to Health may be a better option if you are not sure what intensity or level of care they need, or which services may be best placed to support them.
What is the NWMPHN System of Care?
 The System of Care is NWMPHN’s vision for a person-centred approach to mental health support. Head to Health and CAREinMIND intake teams work within the System of Care to match people with the best available supports according to their specific needs. You can use our System of Care search tool to browse services in our region – including those provided by Head to Health hubs, CAREinMIND providers, and other organisations.
The System of Care is NWMPHN’s vision for a person-centred approach to mental health support. Head to Health and CAREinMIND intake teams work within the System of Care to match people with the best available supports according to their specific needs. You can use our System of Care search tool to browse services in our region – including those provided by Head to Health hubs, CAREinMIND providers, and other organisations.
Shared care survey for GPs
We expect our contracted service providers to work collaboratively with GPs. We have developed a short survey about Head to Health and CAREinMIND to help us understand your experience of shared care with our mental health care providers.
Please take a few minutes to complete the survey.
More information
More information including FAQs for health providers is available at headtohealthvic.org.au
You can also call the Head to Health intake team on 1800 595 212.
Visit the mental health pages on HealthPathways Melbourne for referral information at the point of care.




