
“A key factor in the ability to care for others is the ability to care for oneself.”
General practice plays a central role in the provision of mental health care. In Australia, people in distress frequently turn to a general practice team for help. Mental health remains the most common issue managed by GPs. The latest data show an upward trend, from 61 per cent in 2017, to 65 per cent in 2019 (Health of the Nation Report 2019).
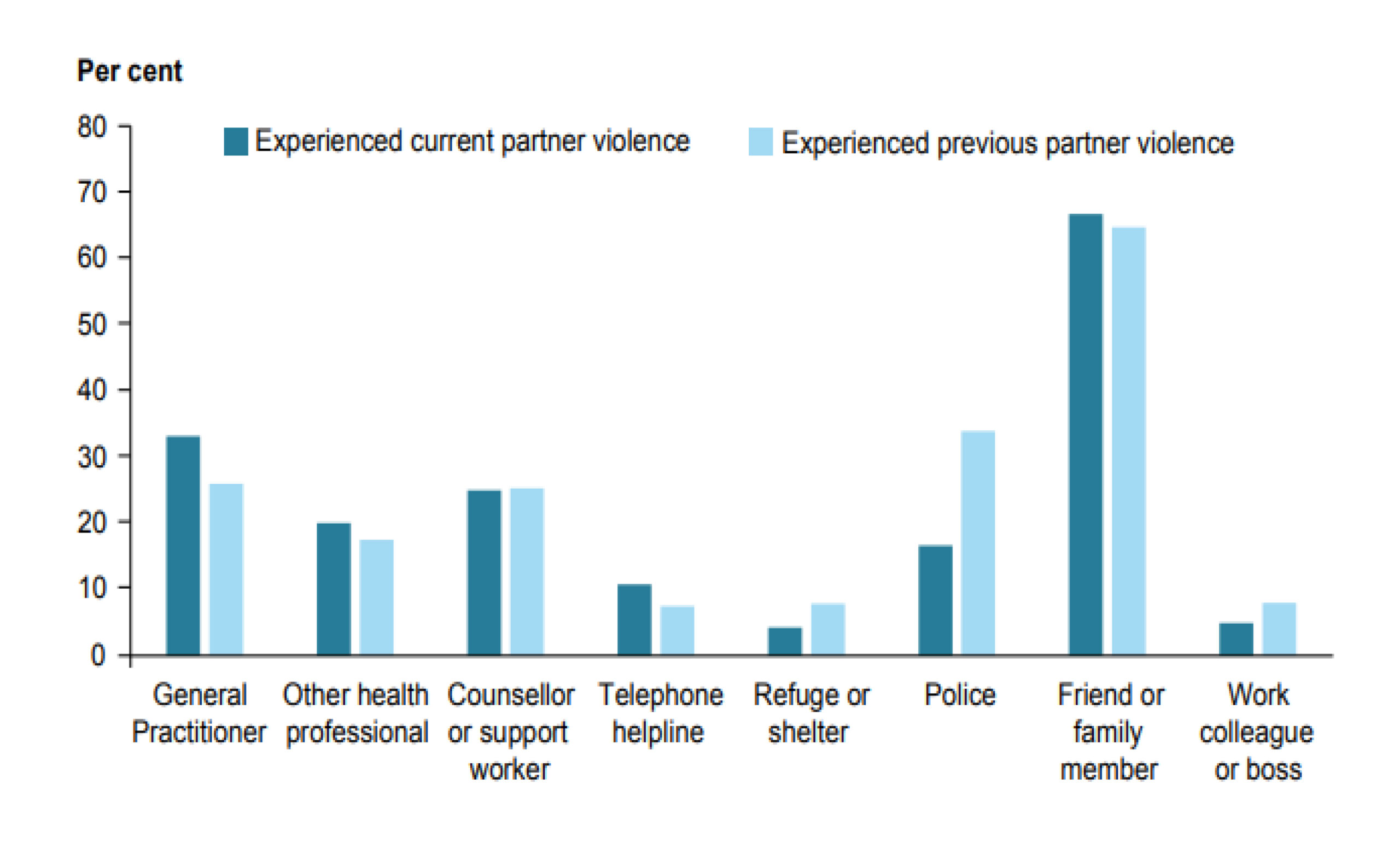
Professor Kelsey Hegarty from the University of Melbourne Safer Families Centre says that after friends and family, victims are most likely to tell their GP or other health professionals about violence. Read on to find out how your practice can work with Professor Hegarty’s team.
Working with patients who are affected by family violence can be difficult and emotionally confronting. Many factors can increase stress for primary health care professionals. These include the emotional impact of hearing survivor stories, the mental and emotional load of caring for these patients, the patient-professional interaction and boundary issues. The long-term nature of the care required also places pressure on GPs and other health care providers.
It is important for GPs to be aware of their own support needs and the strategies they can put in place. The following suggestions can be used at organisational level to prevent and respond to compassion fatigue, burnout, vicarious trauma and secondary traumatic stress.
What can you do to support the practice team?
- Develop a workplace policy that recognises secondary trauma as a potential workplace health risk, addresses related stigma, normalises workplace stress and outlines appropriate responses. These may include including professional development, workload and case management, peer support and ongoing routine management meetings in which secondary trauma is discussed.
- Register for an Employee Assistance Program (EAP). An EAP is an employee benefit program to help employees deal with personal or work-related problems that might adversely impact their work performance, health and wellbeing. The GP Support Program is a free service offered by the RACGP in line with the college’s commitment to foster a culture of self-care among GPs. It is available to all RACGP members regardless of where you live or work. An example of an EAP policy is available to download (.pdf).
- Form in-practice discussion groups to discuss specific cases. One option is to adopt a model of group supervision with a non-medical professional who has experience in counselling and mental health. For example: you may have a psychologist, psychotherapist or mental health social worker attend and facilitate the group. Examples include group supervision in general practice and Balint groups.
- Include family and domestic violence in your HR policy. Develop a HR policy to support employees who experience domestic violence. Provide a workplace environment that promotes their safety and provides the flexibility to support them to live free from violence. As an example, we have made the North Western Melbourne Primary Health Network Family and Domestic Violence Policy (.pdf) available to read.
- Develop a culture of learning, sharing and support within the workplace. Provide support and supervision that includes discussion of secondary trauma and its implications at regular team meetings. This could include:
- Engaging in reflective practice. This can be one-on-one with a trusted friend or your manager, counsellor or other support person, with colleagues, or on your own (for example: by writing in a journal).
- Engaging your team and managers for regular debriefing and other support.
- Offering support and supervision for clinicians working with adult survivors of complex trauma, clinical and non-clinical supervision, case consultation and debriefing, and support for vicarious trauma and self-care.
- Evaluating your workspace to ensure it is conducive to wellbeing. It should have enough space for you and your colleagues to have lunch or chill out together to get away from the pressures of work. Plants, flowers, dashes of colour, natural light, fish tanks and art can also help to brighten the mood.
What resources and support are available?
- New Clinician Self-Care and Caring for Medical Professionals pathways on HealthPathways Melbourne. These provide advice on caring for your own or other medical professionals’ physical and mental health. Although these pathways were written specifically for doctors, they may be useful for other medical professionals.
- Peer support groups. These groups can provide emotional and practical support. Ensure the team is aware of mental health support for practices.
- Complex Trauma Networks offer opportunities to debrief with other professionals and services. They help decrease social isolation by providing a forum for a variety of practitioners to build relationships, exchange knowledge and improve referral pathways. Most networks meet four times a year. Networks in our region include:




