Being able to find, review and interpret data has become essential as practices seek to understand the health needs of their patient population. With these factors in mind, the Health Care Home leaders group met on June 16 for a workshop on the third of Bodenheimer’s 10 Building Blocks – Data Driven (quality) Improvement.
The workshop was co-facilitated by Dr Richard Bills, a general practitioner working in Woodend. Dr Bills has been engaged with the Improvement Foundation of Australia since its inception in 2005 and continues to drive Quality Improvement activities within his practice.
The Leaders Group shared how quality improvement works within their practices including who drives it, who is responsible and how to shift from discrete quality improvement initiatives to building a culture of continuous quality improvement.
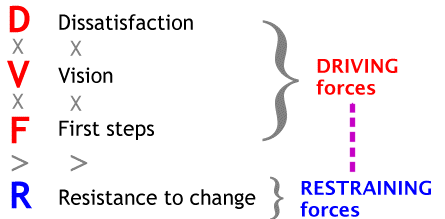
One of the key points discussed was the Beckhard – Harris change equation, which describes the conditions necessary for change to occur. The formula for change (pictured below) is made up of dissatisfaction (D) with the current state, a clear and shared vision (V) of a preferred future, an acceptable first steps (F) roadmap to achieving the vision which together must be stronger than the resistance (R) to change.
This change formula also implies that all three elements on the left side, Dissatisfaction, Vision, and First Steps must be present for change to occur. If any element is missing, change will not occur.
We are now at the six-month mark of the Leaders Group program. Currently the group are working on their quality improvement projects that will move their practices towards adopting the Person-Centred Medical Home (PCMH) model. Along with this, they have also been testing the PCMH self-assessment tool which will shortly be made available to other practices in the region. This tool allows practices to assess their practice against the components of the model in detail and understand where their practice is on the PCMH journey. PHN staff can then support practices to design quality improvement activities around the five areas of the PCMH model:
- Person-centred care
- Coordinated care
- Safe, quality care
- Accessible care
- Comprehensive preventive, acute and chronic disease care
Stay tuned for more information about the PCMH self-assessment tool in July 2018.
If you would like to know more about the PCMH model and how you can adopt it in your practice, please contact Michaela Lodewyckx – Coordinator Primary Care Improvement on michaela.lodewyckx@nwmphn.org.au




