
Changes to the National Cancer Screening Program Clinical Guidelines pathway for women at intermediate risk came into effect from 1 February 2021.
This followed the Cancer Council Australia Clinical Guidelines working party’s review of data from the renewed program.
Why were the changes made?
A review of the national clinical program data was undertaken for women at intermediate risk, whose follow-up test is human papillomavirus (HPV) (not-16/18) positive, liquid based cytology prediction negative, possible low-grade squamous intraepithelial lesion (pLSIL) or low-grade squamous intraepithelial lesion (LSIL).
Results from the review showed that these women will have a low likelihood of histologically-confirmed high grade squamous intraepithelial lesion (CIN2/3) or worse.
Currently, colposcopy clinics are seeing large numbers of women referred for colposcopy, as the proportion of women with persistent infection is higher than predicted.
This demand on colposcopy clinics has meant many women are waiting to see a specialist for extended periods, which can result in increased anxiety. Women at the highest risk (high-grade cytology, HPV 16/18) may be experiencing unnecessary delays for treatment and further clinical investigation.
The new recommendation will:
- avoid the need for many women to have unnecessary colposcopies
- reduce associated harms (biopsy, overtreatment, anxiety and financial costs) for women with HPV‐related cervical abnormalities that would resolve spontaneously without medical intervention.
Refer to the news story and the frequently asked questions on the Australian Department of Health website for more information.
What are the changes?
In summary, a woman is now referred after her third annual non-16/18 HPV positive result in a row, rather than her second as was previously the case (assuming reflex cytology normal or pLSIL or LSIL at worst).
Who is excluded?
Women who may be at higher risk of harbouring a high-grade abnormality should be referred to colposcopy if HPV (any type) is detected at 12 months, regardless of the result of reflex cytology. This includes:
- women two or more years overdue for screening at the time of the initial screen
- Aboriginal and Torres Strait Islander women
- women aged 50–69 years.
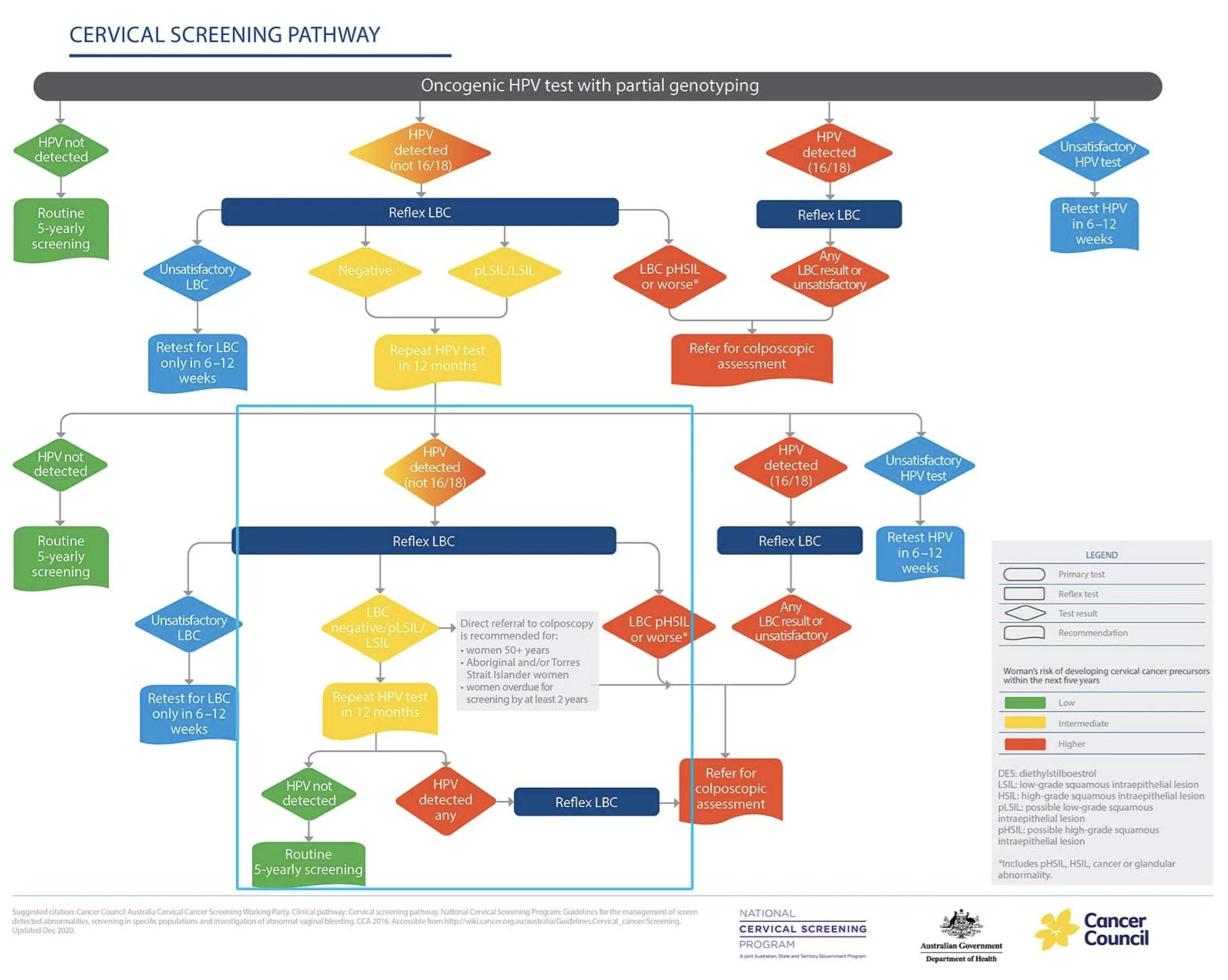
The revised Cervical Screening Pathway flowchart
HealthPathways Melbourne
Visit Cervical Screening on HealthPathways Melbourne for assistance at the point of care. The updates above have been incorporated into this pathway.
Are you a GP or health professional in our region who doesn’t have access to HealthPathways Melbourne? Request access online or contact info@healthpathwaysmelbourne.org.au





