
Why is this important?
Excess weight, especially obesity, is a major risk factor for cardiovascular disease, type 2 diabetes, some musculoskeletal conditions and some cancers.
As the level of excess weight increases, so does the risk of developing these conditions. In addition, being overweight can hamper the ability to control or manage chronic conditions.
What do the statistics say?
- In 2018, 8.4 per cent of the total burden of disease in Australia was due to overweight and obesity.
- In 2017–18, 60 per cent of men and 66 per cent of women had a waist circumference that indicated a high risk of metabolic complications
- In the same period, 31 per cent of Australian adults were obese, up from 19 per cent in 1995.
- In 2019, among 22 OECD member countries, Australia had the sixth highest proportion of overweight or obese people aged 15 years or over.
- For overweight and obesity combined, rates were higher in the lowest socioeconomic areas – recording 28 per cent – compared with the highest socioeconomic areas, where the figure was 21 per cent.
- Emerging research suggests that COVID-19 might have led to weight gain in some cohorts.
Source: Australian Institute of Health and Welfare.
Note: due to the COVID-19 pandemic physical measurements (including height, weight and waist circumference) were not taken at the time of the most recent National Health Survey in 2020–21.
Why BMI?
Body mass index (BMI) is an internationally recognised standard for classifying overweight and obesity in adults. While the measurement is not perfect, at a population level it is a practical, easy and useful.
Recording of BMI status keeps our records up to date and prompts us to have conversations about weight and associated risk factors with appropriate populations. This can lead to evidence-based interventions.
What evidence-based interventions are there for weight management?
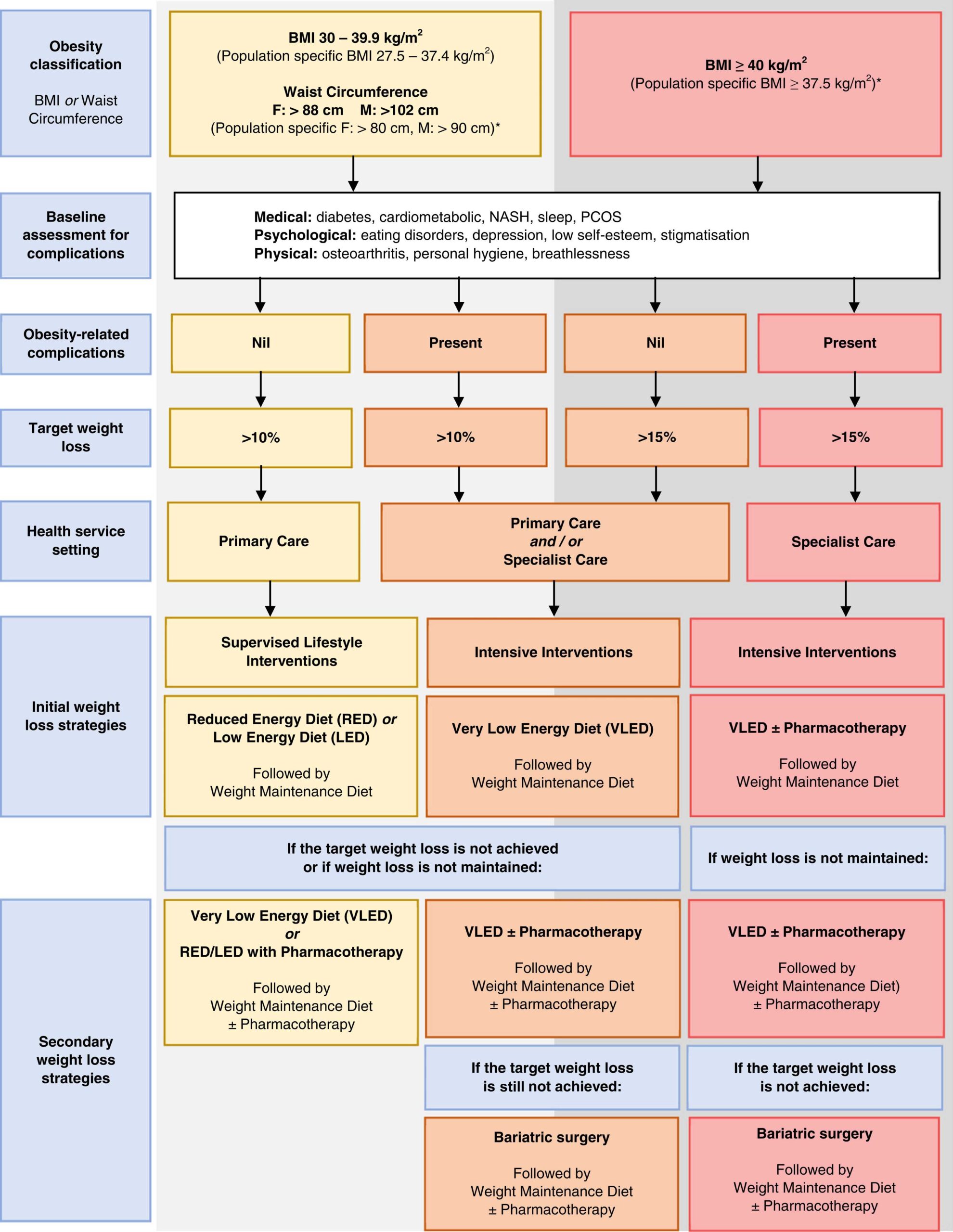
The Australian Obesity Management Algorithm: A simple tool to guide the management of obesity in primary care (2022) is an excellent overview of the evidence-based options for weight loss in Australia. It summarises the guiding principles of weight loss management, including the benefits of weight loss, the role of primary care including identifying assessing and supporting our patients, avoiding weight loss bias and stigma, setting goals and the importance of a person-centred approach. It also includes an excellent algorithm (reproduced below) using BMI and associated risk factors to target treatments.
Evidence based options include:
- Reduced energy intake
- Increased energy expenditure
- Pharmacotherapy (including an overview of the TGA approved options available in Australia and off-label options)
- Surgery
How can PIP QI reports help manage obesity?
North Western Melbourne Primary Health Network (NWMPHN) is continuing to provide individual quarterly PIP QI reports for any general practice in the region wanting to use data to drive improvement.
These reports are based on the 10 measures for the Practice Incentives Program Quality Improvement Incentive.
Remember: you can choose any area of data-driven quality improvement for the PIP QI Incentive, as long as you are working in partnership with NWMPHN. However, the 10 measures have been chosen as evidence-based measurements and are the ideal starting point for a QI activity.
In this article we are taking a closer look at PIP QI Measure 3: Proportion of regular patients aged more than 15 with a BMI recorded in the last 12 months.
How good are we at recording this now?
In the latest data collected in the NWMPHN catchment, 17.7 per cent of patients had a BMI recorded within the past 12 months. If the ideal rate is 100 per cent, how do you feel about this result?
Now, look at your own report.
- How do you compare to the NWMPHN average?
- How do you feel about your result? Is it higher or lower than you expected?
- What are the factors unique to your practice that you think influences the result?
Is 100 per cent ever achievable? Discussing weight can be a sensitive topic. What is a good target to aim for? Think about what is achievable at your practice.
Set a goal
Plan
Make a plan for how you are going to improve your BMI recording rates. An important step in making changes is to have an overall goal to work towards, with a definable measure.
Goal
For example, your practice may aim to improve the proportion of active patients with a BMI status recorded from 60 to 70 per cent.
Measure
Percentage of active patients with a BMI status recorded at baseline and 6 months after making changes.
Tips to improve the recording of BMI at your practice
As a team
- Consider a team meeting and education session. Discuss correct recording (‘coding’) of weight and height information with clinical staff members. Make sure everyone knows how to put the data in the correct area of the software and how to code it correctly. Note: responses that are written in the progress notes are not able to be considered recorded.
- Brainstorm ideas in your team to help improve BMI recording. You might form a project team.
- Discuss the clinical practice guidelines.
Around the practice
- Install This helps by highlighting which patients do not have their BMI status recorded.
- Include height and weight recording on new patient registration forms. Have a process in place for who translates the data into the clinical file.
- Conduct targeted blitzes in your practice to increase recording of BMI status. For example: you could print some cards for reception to hand out that say “This month we are updating everyone’s BMI status. You will be asked in your consultation if your BMI is recorded and up to date.”
- Designate a particular day each week to focus on it. For example: ‘Weight and Height Wednesdays.”
- If your practice nurse has time, they might see patients while they are waiting for the GP, to record their height and weight.
Do it, study it, and act on any changes you want to make
The final step of the Plan, Do, Study, Act (PDSA) cycle is to do what you planned to do: test the ideas, study and reflect on what happened, and make any changes that can continue to improve your work.
For example: you might find that some patients were challenged by the card handout and instead preferred a more personalised approach.
More information
NWMPHN has developed QI Activities which can assist you in tackling improvement in this measure. More information on our quality improvement program and QI activities is available on our website.
- QI Activity – improving BMI recording in your practice
Details on how to use the PIP QI reports is available on the Pen CS website and on our fact sheet (.pdf).
If you have any questions about quality improvement, please contact us on (03) 9347 1188 or email primarycare@nwmphn.org.au
HealthPathways Melbourne 
Visit the Management of Overweight and Obesity in Adults page on Health Pathways Melbourne for assistance on how to assess and manage obesity within your practice.
Are you a GP or health professional in our region who doesn’t have access to HealthPathways Melbourne? Request access online or contact info@healthpathwaysmelbourne.org.au




