
While the Mornington Peninsula continues to be the focus of attention, Buruli ulcer notifications in Melbourne’s northern and eastern suburbs are significantly higher than anywhere else in Victoria, and appear to be rising.
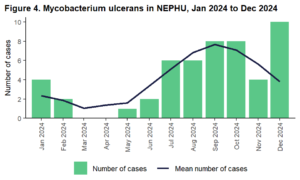
Data provided by the North Eastern Public Health Unit (NEPHU), which covers local government areas from Hume to the Yarra Ranges, reveals higher than expected notifications for the ulcer, which can affect skin and sometimes bone and can lead to permanent disfigurement and long-term disability.
NEPHU numbers for December 2024 show a notification rate of 6.6 per 100,000 people, compared to 4.6 for the state as a whole.
What is a Buruli ulcer?
Buruli ulcer (sometimes called Bairnsdale ulcer) is a skin infection caused by the bacterium Mycobacterium ulcerans. It usually presents as a slowly developing painless nodule or papule which can initially be mistaken for an insect bite.
Over time the lesion can progress to develop into a destructive skin ulcer.
There is increasing evidence that both mosquitoes and possums play a role in transmitting M. ulcerans to humans in Victoria. Prevention measures include reducing mosquito breeding sites, avoiding mosquito bites, covering cuts and abrasions when outdoors, and washing soil and water off contaminated skin.
Early diagnosis is critical
Early diagnosis is critical to prevent skin and tissue loss. Consider the diagnosis for patients with a persistent ulcer, nodule, papule, or oedema and cellulitis, especially on exposed parts of the body.
Where is Buruli ulcer an issue in Victoria?
According to the World Health Organisation, Buruli ulcer is found in at least 33 countries, in Africa, South America and the Western Pacific.
In Australia, the disease is present in Far North Queensland near the Mossman area, the Northern Territory, and in an increasing number of locations in Victoria, both coastal and inland.
The disease can affect individuals of any age, but in Victoria notifications are most common among those aged 60 years and older.
The highest risk is associated with the active transmission areas of Rye, Sorrento, Blairgowrie and Tootgarook on the Mornington Peninsula. There is also moderate risk associated with parts of the Bellarine Peninsula (Ocean Grove, Barwon Heads, Point Lonsdale, Queenscliff), Frankston and Seaford areas.
There is a lower risk associated with the rest of the Bellarine and Mornington peninsulas, the south-eastern bayside suburbs and East Gippsland.
However, since 2019 the disease has been spreading inland. Cases have been reported in:
- Aireys Inlet and the Surf Coast
- Several suburbs of Greater Geelong, in particular Belmont, Highton, Newtown, Wandana Heights, Grovedale and Marshall
- Inner Melbourne suburbs of Essendon, Moonee Ponds, Brunswick West, Pascoe Vale South and Strathmore.
What is the clinical presentation?
There is a relatively long incubation of four weeks to nine months, with a median of four to five months. It usually presents as a non-healing ulcer by the time the patient seeks GP care.

Early diagnosis is critical to prevent skin and tissue loss. Consider the diagnosis in patients with a persistent ulcer, nodule, papule, or oedema and cellulitis especially on exposed parts of the body.
The first sign of Buruli ulcer is usually a painless, non-tender nodule or papule. It is often mistaken for an insect or spider bite and is sometimes itchy. The lesion may occur anywhere on the body, but it is most common on exposed areas of the limbs. In one or two months the lesion may ulcerate, forming a characteristic ulcer with undermined edges.
How is Buruli ulcer diagnosed?
Two swabs (dry, or pre-moistened with sterile saline) from beneath the undermined edges of the lesion should be sent for staining for acid-fast bacilli (AFB), polymerase chain reaction (PCR) and culture. It is essential that there is visible clinical material on the swab.
Treatment
- Refer urgently to an infectious diseases specialist experienced in managing Buruli ulcer or seek advice on the initial management and assessment of all confirmed or highly suspicious cases:
- for initiation and supply of antibiotics in confirmed case of M. ulcerans infection
- if suspected paradoxical reaction (immune reconstitution syndrome) to antibiotic treatment
- to assess if surgery is indicated.
- Wound management: consider referral for specialist wound assessment to assist in wound management.
- Notify Victorian Department of Health within five days of diagnosis of any cases of M. ulcerans.
For more information:
- Victorian Department of Health: Buruli ulcer (Mycobacterium ulcerans infection)
- Better Health Channel: Buruli ulcer
- HealthPathways Melbourne: Buruli Ulcer
- HealthPathways Melbourne: Non-acute infectious diseases referral




