The Preventing Chronic Disease through Quality Improvement project is a 12-month initiative running in practices in the North Western Melbourne Primary Health Network (NWMPHN) region.
The project aims to build capacity in general practices for recognising and recording chronic disease and cancer risk factors. Practices are also implementing initiatives to prevent chronic disease including nurse-led clinics and behavioural lifestyle modification programs (such as exercise programs).
Participating general practices can nominate their own chronic disease prevention activity. Activities can be based on local needs, or a gap in services provided by the practice informed by the improved data quality in the practice.

Melville Medical Group in Pascoe Vale is one of five general practices participating in the project. Karlene Jeffery is both the practice manager and a nurse at the practice. We asked Karlene about the osteoporosis intervention that their practice has completed as part of the project.
Melville Medical Group used the REFRAME Program as part of Pen CS CAT4 and identified more than 421 patients over the age of 70 years who are at risk of osteoporosis. The REFRAME data report uses filters and clinical information to select the following patients of interest:
- Patients over 70 years who have never had a bone density (DEXA) scan
- Patients who have not been scanned in the last two or five years
- Patients who have experienced a fracture since the age of 50
The practice then investigated local service providers that can perform DEXA scans. They found MeasureUp, which provides a free mobile van onsite for DEXA scanning and bulk billing for patients over 70 years.
Ms Karlene Jeffrey: “We chose to look at osteoporosis as we have a regular older patient group and looking at the data showed many were either under screened or not screened at all.
“We recalled patients with a letter as our older demographic group of patients respond well to mail outs. We found they were more engaged when they attended specifically for the issue of bone density rather than an add on to the normal consult. We also found that patients were more likely to agree to have the test done if done onsite rather than a radiology facility.”
The practice identified 421 patients at risk and conducted 170 DEXA scans. This equates to a 40.6 per cent uptake of patients screened, which is almost double the MeasureUp average patient uptake per practice of 20–25 per cent. Of the patients screened, 68.2 per cent were found to have a confirmed diagnosis of either osteopenia (79) or osteoporosis (37).
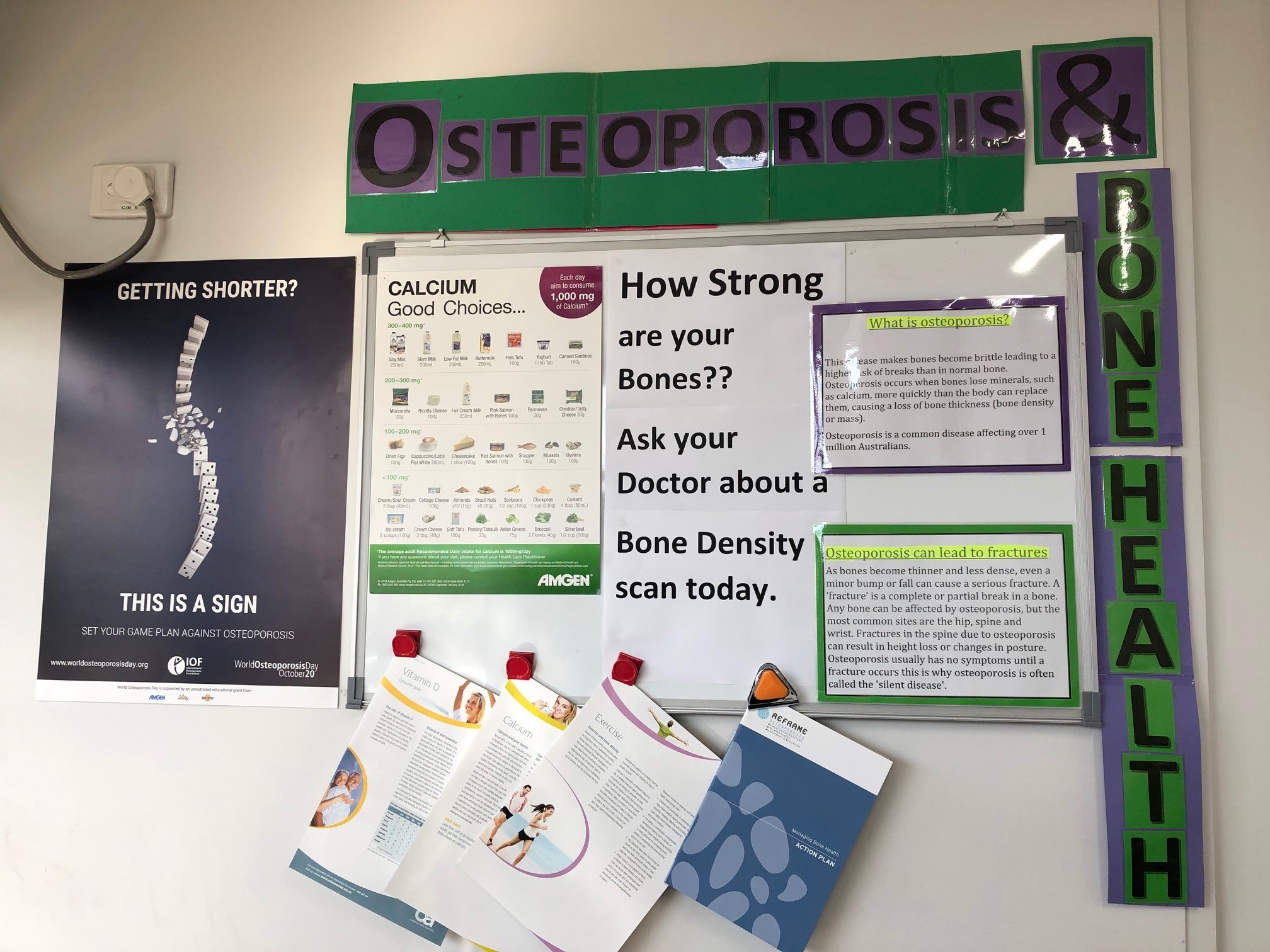
Ms Karlene Jefferey: “We learnt that we needed to upskill our nurses and doctors in diagnosis/care and management of osteoporosis prior to commencing the project. We had practice education sessions run onsite by an osteoporosis nurse educator both for the whole team and one-on-one training for GPs and nurses. We also made sure we had information for patients in the waiting room and on our website.
“Going forward we plan to approach osteoporosis in a systematic way. We have now set up regular recalls and have added a screening question to 75+ health assessment template.
“We also have a regular booking with Measure up to enable easy access for patients and to help to catch those people who turn 70.
“Overall, we feel the project went well and feedback from patients has been positive. We believe it was successful because we planned, upskilled, and put in extra resources, including extra practice manager, doctor and nurse hours all before we commenced. We would consider a slightly different time of year as we found many people were away. We are still getting people attending now.”
How can I implement quality improvement in my practice?
NWMPHN has developed a Quality Improvement Guide and Tools, which includes templates and examples to help you understand how to complete quality improvement activities in your practice.
Your NWMPHN relationship manager can also support you with quality improvement activities. If you would like to discuss quality improvement either contact your relationship manager directly or contact NWMPHN on (03) 9347 1188 or email primarycare@nwmphn.org.au.
Where can I get more information?
HealthPathways Melbourne provides clinical advice and easy-to-follow information about referral services. HealthPathways has the following pages that you may find useful:
If you do not have access to HealthPathways, please contact info@healthpathwaysmelbourne.org.au.
Do you have an interest in osteoporosis?
NWMPHN is seeking GPs, nurses and practice managers who have an interest in osteoporosis to help us develop and deliver education, mental HealthPathways and quality improvement resources for general practice. If you have an interest in osteoporosis please contact primarycare@nwmphn.org.au
Disclaimer: This article was provided by NWMPHN. While every effort has been made to ensure the information is accurate, North Western Melbourne Primary Health Network does not warrant or represent the accuracy, currency and completeness of any information or material included within.




