By Dr Jeannie Knapp, GP and Primary Health Care Improvement GP Adviser, North Western Melbourne Primary Health Network.
We are all biased
The recent, worldwide Black Lives Matter protests have focused our attention on the lived experiences of people of diverse backgrounds. While some discrimination is overt and explicit, much of it is driven by unconscious bias.
All humans harbour unconscious biases – the subconscious associations that cause us to have feelings and attitudes about other people based on characteristics such as race, ethnicity, age, gender, sexuality and appearance. These associations develop over the course of a lifetime, beginning at a very early age through exposure to direct and indirect messaging.
Our unconscious biases tend to preference our own ‘in-groups‘ and can make it very difficult for those in dominant social groups to truly understand the experience of minority social groups.
Why does this matter?
Almost without exception, members of minority subgroups experience worse health outcomes. While some of this can be explained by factors outside of the health system, access to fair and equitable health care is also a contributing factor.
Some examples of poorer health outcomes include:
- For the Aboriginal and Torres Strait Islander population born in 2015–2017, life expectancy was estimated to be 8.6 years lower than that of the non-Indigenous population for males (71.6 years compared with 80.2) and 7.8 years for females (75.6 compared with 83.4).
- Australia’s 2018 Health Report showed that LGBTIQ people face disparities in terms of their mental health, sexual health and rates of substance use. Adults who identify their sexual orientation as homosexual, bisexual or not sure/other report higher levels of psychological distress than heterosexual adults. There is evidence that LGBTIQ people are at a higher risk of suicidal behaviours and have the highest rates of suicidality compared with any population in Australia.
- In 2007–08, almost half (46 per cent) of Australians aged 15–64 years with severe or profound disability reported poor or fair health, compared to 5 per cent for those without disability. People aged under 65 years with severe or profound disability had a higher prevalence rate of all types of selected long-term health conditions than people without disability. Almost half (48 per cent) of people with severe or profound disability had mental health problems, compared to 6 per cent of people without disability. About 42 per cent of people aged 16–64 years with severe or profound disability had seriously thought about committing suicide, including 18 per cent who had attempted suicide.
- According to the North Western Melbourne Primary Health Network Needs Assessment Report (December 2019), recent humanitarian arrivals are likely to have experienced trauma and may require additional mental health support. No specific data exist on the incidence of mental illness in the refugee community in the NWMPHN region. However, current research highlights strong linkages between poor mental health and people experiencing displacement and trauma associated with refugee status.
What is cultural safety?
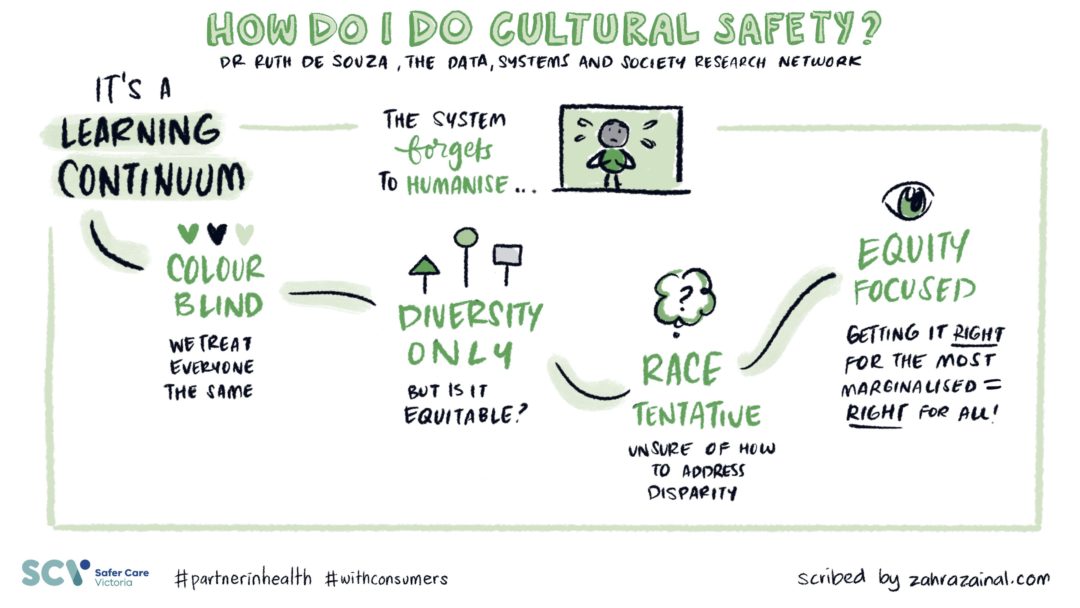
Cultural safety is a term used to describe a way of working with people of different backgrounds that does not diminish demean or disempower them. A person should feel safe to talk about their own unique world views and cultural values without feeling less important than others. Cultural safety is a way of working rather than specific knowledge about cultures. Source
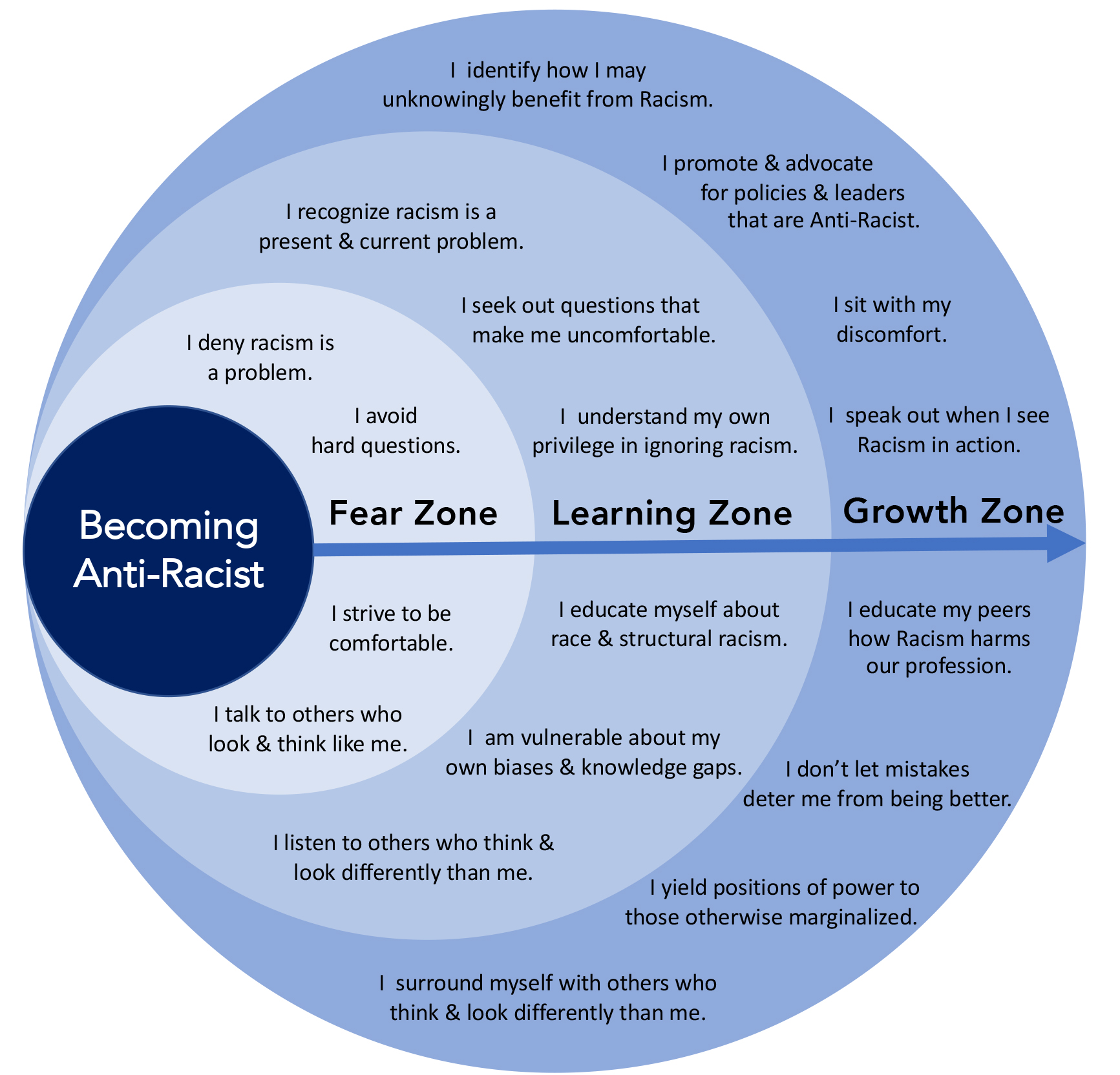
This includes the ongoing critical reflection of health practitioner knowledge, skills, attitudes, practising behaviours and power differentials. In order to do this, we have to become aware of some of our unconscious biases.
How can I address this in my practice?
Providing a welcoming, inclusive non-judgemental space can make people from diverse backgrounds feel more comfortable attending your practice and more likely to seek appropriate health care. Here are some things that you might consider to make your practice more welcoming:
Understand your population:
- Use PEN CAT to understand aspects of your practice. For example: How many Aboriginal and Torres Strait Islander patients your practice has, and the age and gender split.
- Know your local community by referring to the NWMPHN Needs Assessment Report or the 2016 Census QuickStats data to become aware of populations that we may not routinely collect data on. For example: LBGTIQ patients, specific ethnic or CALD groups.
Provide information appropriate for your diverse population. For example:
- Posters, pamphlets, and patient information in community languages.
- Notices welcoming diverse populations. For example: a rainbow flag welcoming LBGTIQ patients or a flyer advertising the languages that different staff members speak.
- Aboriginal and Torres Strait Islander flags.
Provide training for staff:
- Cultural safety training such as that offered by the Victorian Aboriginal Community Controlled Health Organisation.
- Other training specific to the populations in your practice, such as inclusive practice training for a better experience for LGTIQ people.
- How to use language to empower clients and reinforce a person-centred approach for alcohol and other drug clients.
- Use resources from the Centre for Culture, Ethnicity and Health.
- Refugee and asylum seeker health modules available through practicecoaching.com.au
Have relevant policies and procedures that:
- Include mandatory training for all team members, such as cultural safety training.
- Include a zero-tolerance policy for any vilification.
- Empower your team to challenge non-inclusive practices.
Access interpreters for CALD populations:
- It is important to use a qualified interpreter rather than family members. Family members may become emotionally distressed at receiving upsetting medical news and may incorrectly interpret information or become unable to continue interpreting. Family members are also inappropriate when interpreting sensitive information.
- All medical practitioners have access to free telephone interpreting services. Register with the Translating and Interpreting Service (TIS National) to access free interpreter.
- The National Doctors Priority Line is a free phone and face-to-face interpreting service for medical practitioners in private practice. It is available 24 hours a day, every day of the year on 1300 131 450.
Identification of Aboriginal or Torres Strait Islander people in general practice
Resources
This information provides support to practice staff on how to ask all patients about their Aboriginal and Torres Strait Islander status:
Education materials for Medical Director, Best Practice and Communicare clinical and billing software:
This is a CAT 4 Recipe can extract who is identified as Aboriginal and Torres Strait islander in your clinical software. This recipe also goes on to see who is eligible for the PBS Co-payment measure:
Education and training





