The National Mental Health eReferral Prototype Project addressed long-standing challenges in manual referral workflows, disconnected systems, and limited visibility between general practice and mental health intake teams. This initiative demonstrates how PHNs can work together to deliver innovative digital solutions that improve access to services and strengthen coordinated care. The project was funded by the Department of Health, Disability and Ageing (DHDA) and led by NMWPHN with PHNs across Australia.
The challenge was to build a system that delivered faster, more accurate referrals, ensured secure data transfer and ultimately improved mental health outcomes. A key aim was to develop a solution that could be adopted nationally, rather than each PHN creating their own separate systems. Core values guiding the project were standardisation, interoperability, efficiency, ease of use, and a seamless user experience.
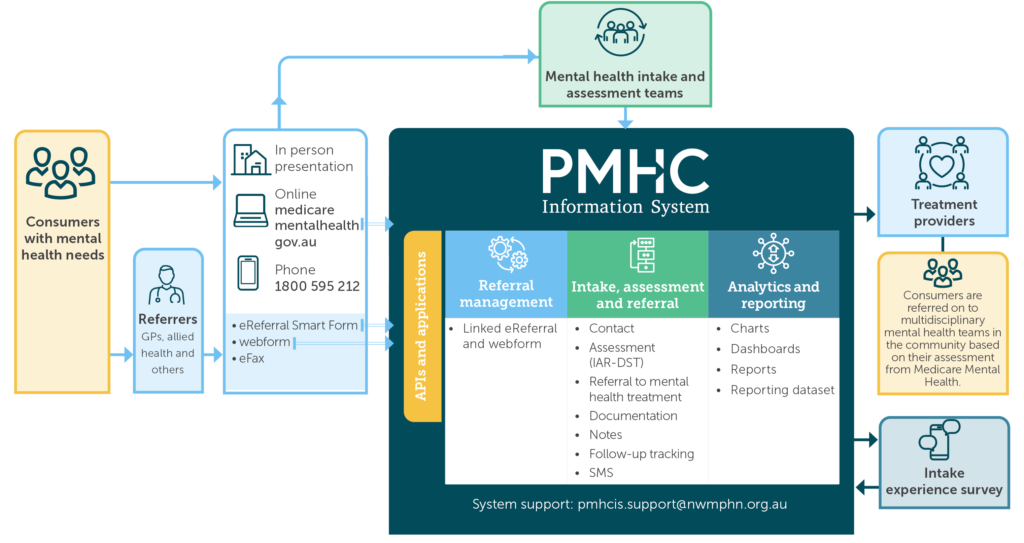
Over 12 months, the project delivered a suite of digital tools, including a HealthLink SmartForm, a back end eReferral Manager, a new eReferral Inbox within the Primary Mental Health Care Information System (PMHCIS), a referral tracking function, and an external webform. The challenge was to build a system that delivered faster, more accurate referrals, ensured secure data transfer and ultimately improved mental health outcomes. A key aim was to develop a solution that could be adopted nationally, rather than each PHN creating their own separate systems.
A core strength of the project was the strategic collaboration between PHNs, HealthLink, intake teams, service providers and national advisory bodies. The Project Advisory Group (PAG) had representatives from 28 PHNs. It and the Expert Advisory Committee (EAC) ensured diverse clinical, technical, and operational perspectives were embedded into every phase of the project, resulting in a solution grounded in real-world service delivery and positioned for future national implementation.
The new system underwent alpha and beta testing – involving three and nine PHNs respectively. This allowed for early testing, iterative improvements, and practical insights into system performance. Evaluation through surveys and interviews with general practitioners (GPs) and intake teams and PHN mental health leads demonstrated clear efficiency gains, and a reduced administrative burden.
Read the report here (.pdf)